Beyond Pharmacotherapy: Understanding the Links Between Obesity and Chronic Mental Illness
While differences in weight-gain potential exist, both between and within classes of psychiatry medications, most commonly used atypical antipsychotics, mood stabilizers, and antidepressants result in some degree of weight gain. This is not new information and it requires an understanding of the tolerability profiles of different treatments and their goodness of fit with specific patient phenotypes. However, this iatrogenic association represents only a piece of this obesity–mental illness dyad. The complex interplay between psychiatric illness and weight involves neurobiology, psychology, and sociological factors. Parsing the salient variables in people with mental illness is an urgent need insofar as mortality from physical health causes is the most common cause of premature mortality in people with chronic mental illness. Our review examines issues associated with common chronic mental illnesses that may underlie this association and warrant further study if we hope to clinically intervene to control this life-threatening comorbidity.
Can J Psychiatry. 2012;57(1):5–12
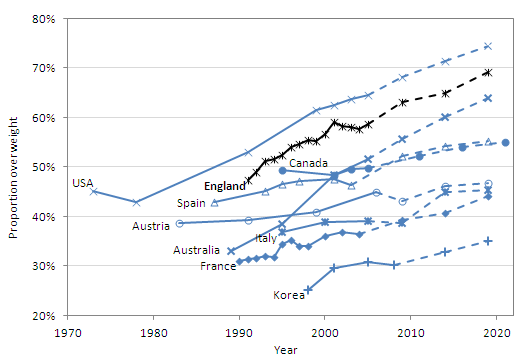
孫銘聰醫師comment: 肥胖在精神病的藥物治療上會影響到體重,有許多的藥物會增加體重,雖然也有些會減少體重,這已經不是新聞,但是精神疾病本身與肥胖也是很有關係,根據本篇回顧性文章,肥胖的問題,在60%躁鬱症患者身上,70%的精神分裂症患者,與55%憂鬱症患者上可以見到此問題。而目前有研究指出睡眠周期受到阻礙,除了在精神性疾患上造成許多患者困擾外,也影響了瘦素(leptin),使得瘦素有了阻抗,無法發揮應有的效用,使得原本應該瘦素有使人在吃完食物後有飽足感的,受到影響後則沒辦法有飽足感。另外睡眠周期受到阻礙,也使得胃泌素(ghrelin)分泌增加,而胃泌素的作用是在刺激食慾,所以這也使得人的食慾在睡眠周期受到阻礙後會增加分泌,進而胃口大開,吃下更多食物。此外,憂鬱也和血中循環的皮質醇(cortisol)分泌增加有關,而皮質醇本身與體重增加也有關係。最後多巴胺(dopamine)在情感性疾病(mood disorder)與肥胖中都可以看到有分泌量減少的狀況。也因此,在神經、精神與社會經濟因素上,都有著複雜的交互作用,影響了體重與精神病,更與其它會影響心血管疾病的因素也有關,例如血糖失去控制、抽菸等問題。